Brain cancer prediction has emerged as a revolutionary frontier in the fight against pediatric gliomas, offering new hope for better management of this challenging condition. Recent studies reveal that advanced AI tools are improving prediction accuracy for relapse risk, particularly when evaluating multiple MRI scans over time. These innovations in AI in pediatric oncology have the potential to transform the standard of care, allowing for timely interventions and enhanced treatment strategies. With a specific focus on glioma recurrence risk, researchers believe that leveraging advanced cancer imaging and techniques like temporal learning in medicine could lead to significant breakthroughs in patient outcomes. This exciting progress underscores the importance of ongoing research in pediatric glioma treatment and the role of technology in transforming healthcare for young patients.
The field of brain cancer forecasting is witnessing groundbreaking advancements, notably in the realm of pediatric brain tumors. Innovative predictive models that utilize complex algorithms are reshaping the landscape of treatment by assessing the potential for tumor recurrence in young patients. By applying artificial intelligence capabilities, particularly in the context of managing gliomas, medical professionals are now equipped with tools that refine their understanding of patient risks. Furthermore, the implementation of longitudinal imaging studies stands to enhance the effectiveness of therapeutic interventions. With these developments, the approach to pediatric brain cancer care is evolving, promising a future where early detection and personalized treatment plans significantly improve survival rates.
Understanding AI in Pediatric Oncology
Artificial intelligence (AI) has emerged as a revolutionary tool in the field of pediatric oncology, particularly for its ability to analyze complex data patterns that traditional methods may overlook. The capacity to process vast amounts of imaging data, such as MRI scans, enables AI to provide physicians with deeper insights into the progression of diseases, including brain tumors in children. With its predictive capabilities, AI assists healthcare providers in making informed decisions quickly, potentially improving outcomes for young patients battling cancer.
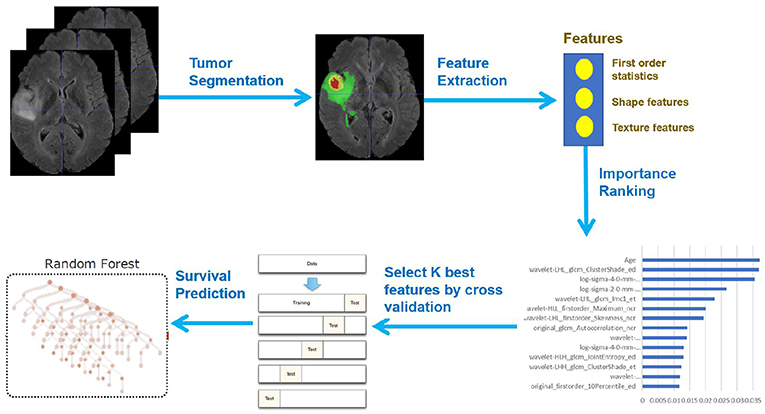
The integration of AI in pediatric oncology extends beyond mere prediction; it actively enhances diagnostic accuracy and tailors treatment pathways for individual patients. Innovations like temporal learning empower AI systems to learn from multiple scans taken over time, which can reveal subtle changes that herald the recurrence of cancer, thus nurturing a more proactive approach to patient care. This marks a significant shift towards personalized medicine in the oncology space, ensuring each child receives the specific treatment they require.
The Role of Temporal Learning in Cancer Predictions
Temporal learning represents a groundbreaking approach in the realm of medical imaging, particularly in predicting cancer recurrence risks. Unlike traditional methods that rely on single snapshots of a patient’s condition, temporal learning leverages sequential imaging data to build a more comprehensive understanding of tumor behavior over time. This methodology is crucial in analyzing brain cancer conditions like gliomas, where the nuances of disease progression can significantly influence treatment strategies.
By utilizing temporal learning, researchers have demonstrated that AI can achieve a predictive accuracy of 75-89 percent in identifying the recurrence of both low- and high-grade gliomas within a year following treatment. Such advancements not only enhance the understanding of glioma recurrence but also pave the way for developing targeted treatment interventions. This can lead to less frequent imaging for patients identified as low risk, thereby reducing their treatment burden and the associated psychological stress.
Catching Brain Cancer Early: The Importance of AI
Timely detection of brain cancer recurrence in pediatric patients is critical for improving treatment outcomes. The innovation brought by AI technologies empowers healthcare professionals to predict relapse risk with a significantly higher degree of accuracy than conventional methods. As research from institutions like Mass General Brigham indicates, AI tools trained on temporal data sets can discern subtle variations between brain scans, crucial for early identification of possible relapses.
This proactive detection not only enhances the therapeutic efficiency but can also alleviate the emotional toll on families who are often under considerable stress during the lengthy follow-up periods with traditional imaging. By focusing on personalized care through improved predictive models, the healthcare system can transition towards more informed and responsive treatment plans that adapt to individual patient needs.
The Future of Pediatric Glioma Treatment
As research continues to evolve, the future of pediatric glioma treatment looks promising with the application of advanced AI technologies. A key focus remains on not only improving predictive accuracy regarding recurrence but also tailoring therapeutic approaches that best suit the patient’s specific cancer profile. With ongoing studies aimed at validating the efficacy of AI-driven predictions, there is hope for more refined treatment modalities that can potentially revolutionize care for young glioma patients.
Moreover, integrating AI into treatment protocols could lead to more efficient resource allocation within healthcare settings. By identifying patients at higher risk for relapse, medical teams can prioritize their care effectively, possibly introducing earlier interventions or modifying treatment plans as necessary. This advancement is a significant step towards holistic care that emphasizes not just survival, but the quality of life for pediatric cancer patients.
Combining Advanced Cancer Imaging with AI Capabilities
The intersection of advanced cancer imaging techniques with AI capabilities is truly reshaping how pediatric oncology is approached today. By enhancing the detail and clarity of imaging modalities, advancements allow AI algorithms to extract critical insights that inform patient care. MRI scans, for example, provide a wealth of visual information; when analyzed through the lens of AI, they can reveal telling signs of tumor behavior and changes over time more accurately.
These developments in advanced imaging, coupled with AI’s analytical prowess, not only aid in predicting recurrence but also in formulating a solid base for clinical decision-making. As physicians harness these tools, they can better understand the dynamics of pediatric gliomas, resulting in actionable insights that effectively tailor treatment to individual needs, ultimately fostering better health outcomes for young patients.
Challenges in AI Implementation in Oncology
Despite the promising advancements in AI and its role in pediatric oncology, several challenges remain in effectively implementing these technologies in clinical settings. One primary concern revolves around the validation and standardization of AI models to ensure they are reliable and applicable across diverse patient populations. Variability in imaging techniques and patient demographics could impact the generalization of AI predictions, necessitating comprehensive studies to ensure robust performance across the board.
Additionally, there are ethical implications and regulatory hurdles that must be navigated when integrating AI into patient care frameworks. The responsibility of ensuring patient data privacy and adhering to medical guidelines remains paramount. As stakeholders in healthcare continue to advocate for AI adoption, it is essential that these challenges are addressed to fully realize the benefits AI can offer in predicting and managing pediatric glioma.
Improving Accuracy in Glioma Recurrence Predictions
Enhancing accuracy in predicting glioma recurrence is not just a matter of improving technology; it involves a multi-faceted approach that incorporates clinical insights and patient-specific factors. The recent findings from studies leveraging AI show significant improvements over traditional methods, but ongoing research is essential to refine these predictions. Implementing machine learning techniques that incorporate clinical variables alongside imaging data could lead to even greater accuracy.
To achieve this goal, collaboration among AI developers, oncologists, and researchers is crucial. By pooling expertise and data from various institutions, the oncology community can work towards models that not only predict recurrence but do so with a nuanced understanding of individual patient contexts. This collaborative effort can potentially set new standards for oncology care and outcomes in pediatric patients.
The Impact of AI on Patient Care Interventions
The potential impact of AI on patient care interventions in pediatric oncology cannot be overstated. As models improve and predictions become more reliable, healthcare providers will be equipped to deliver more tailored interventions for young patients diagnosed with brain tumors. This capability could lead to improved management strategies, such as early therapeutic interventions for high-risk patients and personalized monitoring plans for those identified as low risk.
AI doesn’t just change how we identify potential relapse; it influences the entire care continuum, from diagnosis to post-treatment surveillance. This innovative approach promises to alleviate anxieties frequently associated with prolonged medical follow-ups in children, fostering a more supportive environment for both patients and families during critical times in treatment.
AI and the Future of Pediatric Oncology Research
Looking ahead, the integration of AI into pediatric oncology research holds immense potential for breakthroughs in understanding, predicting, and treating pediatric brain cancer. With ongoing studies indicating that AI can more accurately predict glioma recurrence, the future research landscape will likely see increased funding and focus on AI-enhanced methodologies. As algorithms evolve, more sophisticated models may surface, revealing insights that can transform clinical practice.
Furthermore, as collaboration between AI technologists and medical professionals grows, there will be opportunities to explore new horizons in pediatric glioma treatment and care. This partnership could foster the development of next-generation therapies and intervention strategies that are informed by real-time data analysis, fundamentally changing the approach to care for children battling brain cancer.
Frequently Asked Questions
What role does AI play in brain cancer prediction for pediatric patients?
AI plays a crucial role in brain cancer prediction for pediatric patients by analyzing multiple brain scans over time, which significantly improves the accuracy of predicting relapse risk compared to traditional methods. Researchers have leveraged AI techniques, such as temporal learning, to synthesize findings from numerous MRI scans, enhancing the ability to forecast glioma recurrence.
How accurate is AI in predicting glioma recurrence risk in children?
In studies, AI models utilizing temporal learning achieved an impressive accuracy rate of 75-89% in predicting glioma recurrence risk one year post-treatment. This is a notable improvement over traditional prediction methods based on single scans, which typically offer around a 50% accuracy rate.
What are pediatric gliomas, and why is relapse a concern for brain cancer prediction?
Pediatric gliomas are a type of brain tumor commonly found in children. Although many of these tumors are curable with surgery, the risk of relapse can be a significant concern. Accurate brain cancer prediction, particularly for recurrence, is essential for developing targeted treatment strategies and reducing assessment burdens on young patients and their families.
What is temporal learning in the context of brain cancer prediction?
Temporal learning is a novel AI technique utilized in brain cancer prediction that involves training models to analyze a series of MRI scans taken over time. This method allows for the detection of subtle changes in tumor characteristics, thereby enhancing the model’s predictive capabilities regarding glioma recurrence.
How does advanced cancer imaging improve outcomes for pediatric glioma patients?
Advanced cancer imaging, combined with AI tools, improves outcomes for pediatric glioma patients by providing more precise predictions regarding the risk of tumor recurrence. This better risk stratification can lead to tailored follow-up care and interventions, ultimately aiming to optimize treatment and reduce unnecessary stress and imaging burdens on patients.
What are the implications of AI in pediatric oncology for brain cancer treatment?
The implications of AI in pediatric oncology for brain cancer treatment include the potential to personalize care based on predicted recurrence risks, which can guide more effective use of imaging and intervention strategies. This advancement may lead to fewer unnecessary procedures for low-risk patients while ensuring high-risk individuals receive appropriate follow-up care.
What are the future prospects of AI in brain cancer prediction?
Future prospects of AI in brain cancer prediction include further validation of these predictive models in clinical settings, the launch of clinical trials to test AI-informed risk predictions, and possible applications in various medical imaging contexts where longitudinal data is available. This could revolutionize how brain cancers, particularly pediatric gliomas, are monitored and treated.
| Key Points | Details |
|---|---|
| AI Tool for Relapse Prediction | An AI tool predicts the relapse risk in pediatric brain cancer patients with higher accuracy than traditional methods. |
| Study Significance | The study aims to enhance the care for children with gliomas, improving treatment and reducing unnecessary stress from frequent MRI scans. |
| Research Background | Conducted by Mass General Brigham and partners, utilizing nearly 4,000 MRI scans from 715 patients. |
| Temporal Learning Approach | The AI model was trained to analyze multiple MRI scans over time, not just single images, enhancing prediction accuracy. |
| Model Accuracy | The temporal learning model achieved 75-89% accuracy in predicting recurrence within one year post-treatment. |
| Future Implications | Researchers aim to conduct clinical trials to use AI-driven predictions to optimize patient care. |
Summary
Brain cancer prediction is revolutionized by AI tools that accurately forecast the risk of recurrence in pediatric patients. This innovative approach leverages temporal learning from multiple MRI scans to enhance diagnostic accuracy, potentially changing the treatment landscape for children with gliomas. With the ability to reduce the stress of frequent imaging and provide targeted therapies for high-risk patients, the future of brain cancer care is promising.