CRISPR gene editing represents a groundbreaking leap in biotechnology, offering unprecedented potential to modify the very fabric of life. This cutting-edge gene editing technology not only paves the way for revolutionary treatments, like a potential cure for sickle cell disease, but also invites critical discussions about CRISPR ethics and the implications of genetic manipulation. As innovators navigate the complexities of health equity, the ethical dilemmas surrounding who gets access to these advancements loom large. The transformative promise of CRISPR is shadowed by questions regarding bioethics and gene editing—should we edit the human genome to enhance or eliminate certain traits? As scientists and ethicists grapple with these weighty issues, the future of gene editing technology remains both exciting and fraught with moral uncertainty.
The field of genetic modification has taken a significant turn with the advent of CRISPR technology, a method that allows for precise changes to DNA sequences. This novel approach to gene manipulation is not just about eradicating genetic diseases like sickle cell anemia but also raises intriguing concerns about the responsibilities of scientists and the implications for future generations. The dialogue surrounding gene editing extends beyond mere biomedical advancements to encompass vital discussions around ethical standards and the social consequences of such technologies. As we explore this brave new world of genetic engineering, considerations of health equity and societal ramifications will play a crucial role in shaping public perception and policy. Ultimately, understanding the broader context of these innovations is essential for fostering a responsible approach to the evolution of genetic research.
The Promise and Peril of CRISPR Gene Editing
CRISPR gene editing technology has revolutionized the field of genetics, offering the potential to eradicate several genetic disorders, including sickle cell anemia. This innovation poses a groundbreaking opportunity for pediatric medicine, particularly in how we approach diseases that have caused suffering for generations. However, while the technology holds immense promise, it also invites serious ethical deliberations that we, as a society, must confront. The debate revolves around the fundamental question of whether we should alter human genetics and, if so, under what circumstances.
As highlighted by experts like Neal Baer, the ethical implications of utilizing CRISPR go beyond mere technical capability. Should we correct traits simply because we can? This ponderous question leads us down a path of examining the moral compass that guides decisions about human variation and health. It challenges us to consider who holds the authority to determine the ‘correct’ nature of human life and what consequences arise from these choices.
Ethical Considerations in CRISPR Applications
The ethical dimension of CRISPR gene editing brings to light the need for a rigorous framework that addresses the complexities of gene manipulation. For instance, while many advocate for the application of CRISPR in curing life-threatening conditions, there is hesitation regarding its use for less severe traits, such as cosmetic modifications or enhancements. This creates a slippery slope, prompting the question: where should we draw the line? The involvement of bioethics in gene editing discussions becomes paramount to navigate this uncharted territory.
Additionally, discussions surrounding CRISPR must consider the implications for health equity. As Baer pointed out, the high cost associated with gene therapies, such as a $2.2 million treatment for sickle cell disease, raises concerns about who can access these potentially life-saving treatments. If only a privileged few can afford these advancements, the risk of widening health disparities becomes evident, making it crucial for legislators and stakeholders to prioritize fairness and equity in access to these technologies.
Health Equity and CRISPR Technology
At the heart of the discussion around CRISPR gene editing is the issue of health equity. With breakneck advancements in gene editing technologies, there is a growing concern that benefits could disproportionately favor those with financial resources, leaving marginalized communities at an even greater disadvantage. Experts like Rebecca Brendel emphasize the importance of integrating health justice into the conversation to ensure that innovations in gene editing contribute to reducing disparities rather than exacerbating them.
For gene editing to serve as a tool for social good, frameworks must be established that guarantee equal access and fair treatment for all individuals, regardless of socio-economic status. As CRISPR offers the potential to provide cures for genetic disorders, it is vital that the moral and ethical implications are balanced with practical considerations surrounding accessibility, affordability, and informed consent. Only through such careful consideration can we hope to realize the full potential of CRISPR while safeguarding against its misuse.
Bioethics and the Future of Gene Editing
The rapidly evolving field of gene editing calls for a robust bioethical framework that can address the multifaceted issues arising from its application. As neurobiologist and ethicist Neal Baer suggests, we must systematically evaluate the consequences of gene editing not only from a scientific standpoint but also from a moral perspective. This encompasses the social, cultural, and psychological implications of altering human genes, particularly in heritable forms that impact future generations.
Moreover, bioethics in gene editing also involves discussions about the oversight needed to regulate such technologies effectively. Questions around who gets to decide what constitutes acceptable gene modifications and what standards should guide these decisions are pivotal. The potential for misuse, whether in the form of genetic enhancement or even biowarfare, further complicates the bioethical landscape, necessitating a proactive approach to governance and ethical guidance.
Innovative Treatments: The Sickle Cell Cure
The potential to cure sickle cell disease through CRISPR technology stands as a landmark achievement within precision medicine. This radical approach not only aims to alleviate the suffering of individuals afflicted with the disease but also represents the forefront of innovation in gene therapy. With the ability to make precise edits to the genome, scientists can target the underlying causes of sickle cell anemia, offering hope for millions affected globally.
However, the road to implementing CRISPR as a viable cure is fraught with challenges. Beyond the technical hurdles, the cost associated with treatment poses significant barriers to access. Discussions surrounding the economic implications of gene therapies must align with the ethical need for wide-reaching availability, ensuring that advancements in treatment do not further deepen societal disparities but rather promote enhanced health outcomes for everyone.
Societal Implications of Gene Editing
The societal implications of CRISPR gene editing extend into numerous domains of life, from public health to legal frameworks. As we venture deeper into the era of gene manipulation, society must grapple with how these changes affect our understanding of human identity and variation. The ability to modify genes allows for unprecedented control over biological outcomes, inviting conversations about the morality of ‘playing god’ with human genetics.
Furthermore, the societal narrative surrounding gene editing must include diverse perspectives and voices to ensure decisions do not cater solely to the privileged few. Engaging underrepresented communities in discussions about CRISPR and health equity is crucial to avoid perpetuating historical injustices in healthcare. By fostering an inclusive dialogue, we can better understand the societal impacts of gene editing and work towards solutions that prioritize ethical responsibility and communal benefits.
Gene Editing Technology: Opportunities and Risks
While CRISPR technology presents groundbreaking opportunities to alter genetic destinies, it also comes with a multitude of risks and unknowns. The prospect of editing genes with precision may seem appealing, but the long-term effects and unanticipated consequences remain largely unexplored. As scientists tinker with the blueprint of life, it becomes imperative to consider the balance between innovation and caution, especially when weighing risks that could impact not only individual patients but entire populations.
Additionally, the rapid pace of gene editing advancements could outstrip the creation of adequate regulatory and ethical frameworks. This reality calls for a proactive approach to ensure that scientific innovation does not precede our capacity to understand and manage its implications effectively. As stakeholders in healthcare and science, we must advocate for responsible practices in gene editing that prioritize patient safety while navigating the complex ethical landscape that accompanies such profound capabilities.
The Future of CRISPR: Ethical Governance
Looking forward, the governance of CRISPR technology is paramount to ensure ethical standards are upheld. It will be critical for regulatory bodies to create transparent guidelines that delineate the appropriate use of gene editing, considering both societal norms and scientific advancements. Striking the right balance between facilitating innovation and protecting public welfare will require robust stakeholder engagement, including voices from bioethics, medicine, policy, and the public.
Moreover, as we shape the future of CRISPR and its applications, ongoing research and discourse around its ethical implications will be essential. By maintaining vigilance through ethical discussions alongside technological progress, we can better prepare ourselves for the challenges posed by gene editing, ultimately harnessing its power for the greater good while mitigating possible adverse consequences.
Regulatory Frameworks for Gene Editing
The establishment of comprehensive regulatory frameworks is essential to oversee the application of gene editing technologies like CRISPR. As the technology continues to evolve, there is a pressing need to develop guidelines that address not only safety and efficacy but also the ethical considerations that arise from manipulating genetic material. A proactive regulatory approach can prevent misuse and ensure that the benefits of gene editing are distributed equitably among all populations.
Furthermore, these frameworks need to be adaptable, recognizing that the field of gene editing is both dynamic and complex. Collaboration among scientists, ethicists, and policymakers will be crucial in crafting regulations that can respond to new developments while safeguarding against potential abuses. A focus on transparency and public engagement will also help build trust in the regulatory process and ensure that societal concerns are addressed effectively.
Frequently Asked Questions
What is CRISPR gene editing and how does it work for conditions like sickle cell disease?
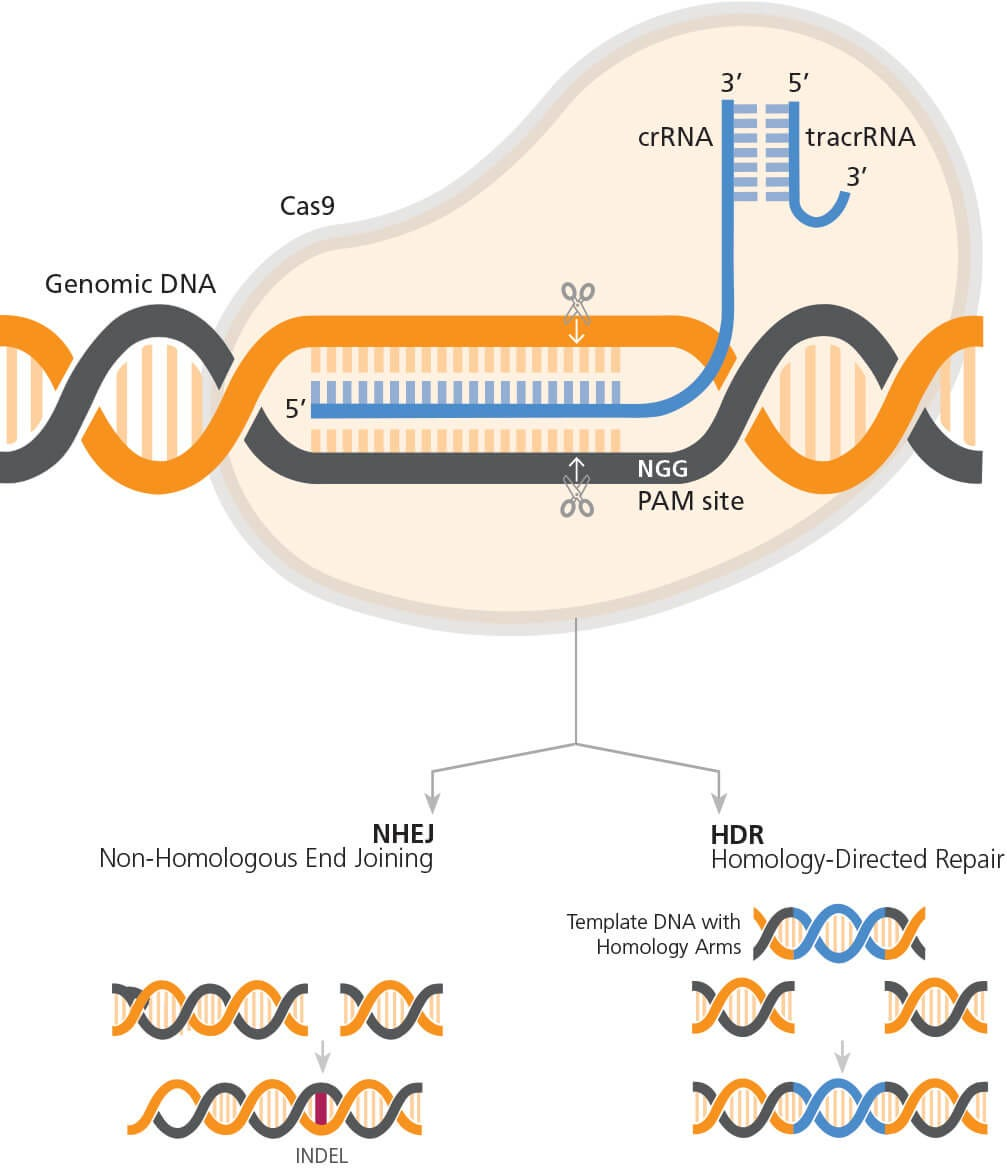
CRISPR gene editing is a revolutionary technology that allows scientists to precisely modify DNA sequences in organisms. It works by targeting specific genes and either cutting them out or altering them. For conditions like sickle cell disease, CRISPR can edit the somatic cells of patients to remove the defective gene, potentially curing the disease. By using this technology, researchers can change the genetic instructions that lead to the symptoms of sickle cell, providing hope for effective treatments.
What are the ethical concerns surrounding CRISPR gene editing technology?
CRISPR gene editing technology raises significant ethical concerns, particularly regarding its application for non-life-threatening conditions. Questions arise about whether we should alter traits that are part of human variation, such as in cases like Down syndrome or hearing loss. Ethical considerations also include health equity, especially concerning the high costs of treatments, which may not be accessible to all individuals, exacerbating disparities in healthcare.
How does CRISPR gene editing relate to health equity and accessibility in medicine?
CRISPR gene editing has the potential to offer life-saving treatments, such as for sickle cell anemia, but its high costs pose challenges to health equity. The price tag for CRISPR-based therapies, often exceeding a million dollars, creates barriers for many patients, particularly in low-income communities. This raises important questions about who can afford these advancements and how we can ensure that all populations benefit from innovative gene editing technologies.
Is CRISPR gene editing a solution for all genetic disorders?
While CRISPR gene editing presents groundbreaking opportunities for treating various genetic disorders, it is not a one-size-fits-all solution. Each genetic condition is unique, and editing can have unintended consequences. For example, altering one gene may affect other critical functions in the body. Therefore, thorough research and ethical considerations are crucial when determining which conditions are appropriate for CRISPR intervention.
Who decides the ethical use of CRISPR gene editing in medicine?
The decision-making process regarding the ethical use of CRISPR gene editing involves multiple stakeholders, including scientists, ethicists, healthcare providers, patients, and regulatory bodies. Discussions focus on balancing innovation with moral responsibilities, as the consequences of gene editing can have profound implications for individuals and society. The goal is to create guidelines that prioritize patient safety, informed consent, and equitable access.
What are the long-term implications of using CRISPR gene editing for biological changes?
The long-term implications of using CRISPR gene editing encompass potential benefits and risks. While it can enable the eradication of genetic diseases, it also raises questions about human enhancement and the ethical landscape of genetic modifications. The possibility of unintended genetic consequences necessitates robust oversight and study to ensure that changes do not adversely impact future generations or disrupt existing ecosystems.
| Key Points | Details |
|---|---|
| CRISPR Gene Editing Explained | CRISPR allows precise editing of genes to potentially cure genetic diseases. |
| Ethical Dilemmas | Debates surround the modification of human traits and the implications for society. |
| Socioeconomic Concerns | Expensive treatments raise questions about accessibility and health equity. |
| Parental Decision-Making | Who decides which traits should be modified in children? |
| Unintended Consequences | Gene editing can lead to unpredictable side effects due to complex gene interactions. |
| Need for Oversight | Without regulations, there could be misuse of gene-editing technologies. |
Summary
CRISPR gene editing presents a revolutionary opportunity in medicine, aiming to cure genetic disorders such as sickle cell anemia. However, it also introduces a myriad of ethical considerations that society must address. From the implications of altering human traits to the socioeconomic factors that influence access to such treatments, the dialogue surrounding CRISPR technology is just beginning. As discussions evolve, it is crucial to find a balance between innovative medical advancements and the broader ethical ramifications they entail.