CRISPR gene editing represents a groundbreaking advancement in biotechnology, allowing scientists to alter DNA with unprecedented precision. This revolutionary CRISPR technology holds the promise of curing debilitating genetic disorders, such as sickle cell disease, which afflicts thousands. However, as we explore these new frontiers, critical discussions around gene editing ethics emerge, raising profound questions about our responsibility toward human diversity. The implications for health equity also weigh heavily, as access to such therapies could be limited, creating disparity among populations. Engaging with medical ethics surrounding CRISPR gene editing is essential as we navigate both its potential and challenges.
Gene modification through CRISPR offers a transformative approach to altering genetic information, inviting a discourse filled with both excitement and apprehension. This innovative editing method could pave the way for significant breakthroughs, particularly in treating hereditary illnesses like sickle cell anemia. Yet, the ethical considerations surrounding gene manipulation cannot be ignored, as we must contemplate the repercussions on natural human variation. Moreover, the topic of health equity raises critical issues, questioning who gets access to these life-changing treatments and at what expense. As we delve deeper into this evolving field, the intersection of science, society, and ethics becomes increasingly important.
Exploring CRISPR Gene Editing: Innovations and Implications
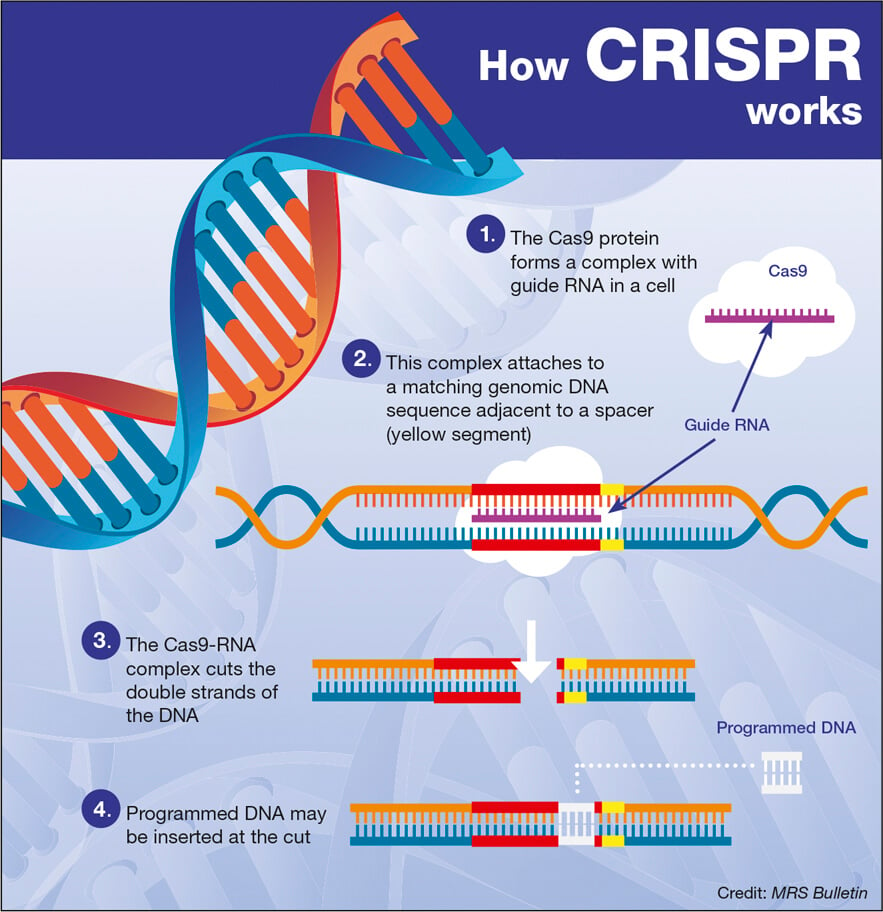
CRISPR gene editing represents a revolutionary leap in genetic technology, enabling scientists to make precise alterations to DNA. This mechanism allows for targeting specific genes that cause diseases, effectively opening the door to potential cures for various genetic disorders, such as sickle cell anemia. However, with great power comes great responsibility, prompting discussions around the ethical implications of such interventions. As we explore the possibilities of CRISPR technology, we must carefully consider the ramifications of altering the human genome and the moral questions that arise with these advancements.
The efficacy of CRISPR gene editing is evidenced by its promise to cure inherited diseases, but ethical dilemmas abound. For instance, while the prospect of eradicating sickle cell disease excites the medical community, it begs the question: is it acceptable to edit human embryos for conditions that, while challenging, are not fatal? Engaging with such scenarios highlights the necessity of overseeing these technologies within the framework of medical ethics to ensure that interventions do not lead to unintended societal consequences that could deepen inequality or stigmatization.
The Ethical Landscape of Gene Editing
Gene editing, particularly through technologies such as CRISPR, intertwines with complex ethical considerations that cannot be overlooked. Discussions surrounding gene editing ethics often reference the potential for enhancement versus therapeutic interventions, and who has the authority to make such decisions. These queries lead to deeper inquiries about individual rights versus collective good, especially when considering the diversities that make up human experience. As pointed out during the recent talk by Neal Baer, the ethical mishaps in determining what constitutes a disease versus a variation are critical and require profound discourse.
Moreover, the ethical landscape is shaped by the consequences of possibly prioritizing certain lives over others, particularly in terms of healthcare access and fairness. As advancements in gene editing come with significant costs—exemplified by the staggering $2.2 million treatment for sickle cell—questions arise about health equity. It becomes vital to ensure that breakthroughs in technology are not just accessible to the affluent but are distributed equitably, reflecting justice in health outcomes. The work of ethical committees and bioethicists is paramount in navigating these murky waters.
Health Equity: Balancing Innovation with Fairness
Health equity involves ensuring that all individuals have a fair opportunity to attain their highest level of health. The advent of CRISPR technology promises breakthroughs but also poses threats to this principle. Given that gene editing can offer life-changing treatments, underserved communities might remain marginalized if these innovations are priced beyond their reach. Hence, initiatives should prioritize not just the development of effective gene editing therapies, but also their affordability, availability, and accessibility to all populations.
Furthermore, addressing health equity challenges requires a concerted effort among policy-makers, healthcare providers, and researchers. Equitable access to CRISPR-derived treatments necessitates systemic changes that can mitigate existing disparities. Baer’s cautionary tale regarding the potential widening of the health gap resonates deeply, urging us to strategize on implementation frameworks that uphold justice and fairness in healthcare. As we move forward, incorporating an equity lens in discussions about technological innovations will be crucial for fostering inclusive healthcare systems.
Medical Ethics: Guiding the Future of Gene Editing
The rapidly evolving field of gene editing raises urgent medical ethics questions that need attention from both practitioners and ethicists. Medical ethics is rooted in principles such as autonomy, beneficence, non-maleficence, and justice, which provide a framework for evaluating the implications of CRISPR technologies. For example, the debate surrounding parental choice—whether it’s ethical for parents to select traits for their children—illuminates the necessity of guided decision-making within the medical community to prevent potential overreach.
Moreover, the recent conversations about oversight in gene editing underscore the critical role of ethical governance. With the possibility of gene editing being performed in countries with lax regulations, the global community must share collective responsibility for ethical standards in research and clinical practices. Establishing international guidelines for CRISPR and similar technologies can help mitigate risks associated with unregulated use and promote safe, ethical advancements in medical science.
Curing Sickle Cell: The Promise and Peril
Curing sickle cell anemia represents a monumental achievement within gene editing capabilities, particularly through CRISPR technology. Advances in this field could transform lives by eliminating the debilitating effects associated with the disease. However, as Baer articulated in his talk, the allure of a cure must be balanced with an awareness of the societal disparities that could be exacerbated by such treatments. While some may receive life-saving therapies, others may be left behind, compelled to navigate the systemic inequities that plague healthcare systems across the globe.
The narrative surrounding sickle cell treatment not only highlights groundbreaking medical advancements but also emphasizes the need for ethical discourse in the context of race and socioeconomic status. With a significant portion of sickle cell patients coming from marginalized communities, the discourse on access and affordability becomes paramount. Ensuring equitable access to these potentially life-altering treatments is essential to avoid reinforcing existing disparities in healthcare.
The Future Pathways of CRISPR and Gene Editing
Looking ahead, the pathways for CRISPR and gene editing technology must be navigated thoughtfully and collaboratively. As the science evolves, so too must our ethical frameworks and regulatory mechanisms—guiding research, clinical applications, and public policy surrounding these innovations. The risks associated with uncontrolled advancements necessitate a proactive approach in educating stakeholders, including researchers, healthcare providers, and the public, about the implications of genetic modifications.
Moreover, the future of CRISPR lies in balancing innovation with rigorous ethical standards—an endeavor that requires engagement from diverse voices within society. From the scientific community to patient advocacy groups, the collective input will be essential in shaping policies that reflect the values of health equity and justice. By prioritizing ethics alongside innovation, we stand to harness the potential of CRISPR to promote health improvements that benefit all, rather than exacerbating inequities.
Understanding Genetic Modification and Its Impact
Genetic modification, especially through technologies like CRISPR, evokes a spectrum of responses regarding its impact on society. While it holds promise for correcting genetic defects and enhancing health outcomes, it also raises fears about the long-term consequences of altering the fundamental blueprint of life. The complexity of genetic interactions means that interventions may produce unintended effects, making it imperative to study these changes thoroughly before applying them in clinical settings.
As advancements in gene editing continue to evolve, stakeholders must prioritize comprehensive impact assessments to weigh the benefits against potential risks. Engaging in public discourse around genetic modification fosters transparency and allows for informed decision-making that includes diverse perspectives. Understanding the science behind CRISPR and its implications is vital for equipping individuals and communities to participate actively in conversations about their future in a genetically modified world.
The Role of Oversight in Gene Editing Technologies
Oversight remains a critical element in ensuring the responsible utilization of gene editing technologies. The legal and regulatory frameworks surrounding CRISPR and similar methodologies must be robust enough to prevent exploitation and unethical applications. The need for international cooperation in establishing guidelines cannot be overstated, particularly as advances in gene editing may occur unregulated in various regions. Without a centralized system of accountability, the risk of misuse, including biological enhancements or genetic discrimination, grows exponentially.
Additionally, organizations that seek to monitor gene editing must encompass diverse stakeholders, including ethicists, scientists, policymakers, and the communities affected by these technologies. Establishing inclusive governance structures allows for a comprehensive evaluation of gene editing, taking into account the lived experiences of populations that may be disadvantaged by such advancements. By emphasizing ethical oversight, we can work towards a future where gene editing benefits humanity equitably and responsibly.
Navigating Future Innovations in Gene Editing
As the landscape of gene editing continues to shift, navigating future innovations should be approached with both excitement and caution. The potential to transform healthcare through CRISPR and related technologies is immense, but so too are the ethical questions that accompany these advancements. Creativity in scientific discovery must be met with equivalent imaginative thinking in policy and ethics to devise solutions that ensure both advancements in human health and adherence to moral principles.
Sustained dialogue among researchers, ethicists, healthcare providers, and communities will be essential for fostering an environment conducive to responsible innovation. This dialogue will help in balancing the exploration of novel gene editing applications while safeguarding against the unintended societal impacts that may arise. By actively engaging a diverse array of voices in the conversation surrounding gene editing, we can pave the way for innovations that are not only groundbreaking but also aligned with our collective values and responsibilities.
Frequently Asked Questions
What are the ethical considerations of CRISPR gene editing?
CRISPR gene editing raises several ethical concerns, especially regarding the alteration of germline cells, which could affect future generations. Questions arise about the rights of individuals versus the potential benefits of eradicating genetic disorders. Important discussions around health equity also emerge, particularly when considering who has access to these technologies and whether they should be used for conditions compatible with life, like Down syndrome.
Can CRISPR technology effectively cure sickle cell disease?
Yes, CRISPR technology shows promise in curing sickle cell disease by editing the genes responsible for the disorder in somatic cells. This gene editing has resulted in successful treatments for individuals, but it comes with a high cost, raising concerns about health equity and access for all patients affected by the disease.
What is the role of health equity in CRISPR gene editing applications?
Health equity plays a crucial role in the discussion of CRISPR gene editing applications, particularly in how access to such advanced treatments may not be available to all populations. The ethical implications of who receives these therapies and the potential for widening health disparities must be carefully considered as gene editing becomes more mainstream.
How does CRISPR gene editing challenge traditional medical ethics?
CRISPR gene editing challenges traditional medical ethics by introducing questions regarding the moral responsibility of altering human genetics. These changes can lead to unintended consequences and raise issues about consent, especially for unborn children. The ability to make decisions on characteristics and potential ‘improvements’ can complicate our understanding of what is considered a ‘normal’ human variation.
What potential risks does CRISPR gene editing pose to future generations?
CRISPR gene editing poses potential risks to future generations by altering germline DNA, which can lead to unforeseen genetic consequences. As genes interact in complex ways, the long-term effects of these alterations are not yet fully understood, raising concerns about the safety and ethical implications of editing heritable genetic traits.
What are the implications of using CRISPR gene editing for non-life-threatening conditions?
Using CRISPR gene editing for non-life-threatening conditions raises ethical dilemmas about the justification for such interventions. The discussion includes whether parents should be allowed to select traits for their children and the societal implications of designing human beings based on preferences, which challenges the notion of genetic diversity.
How do scientists ensure the safety of CRISPR technology in medical applications?
To ensure the safety of CRISPR technology in medical applications, rigorous research and clinical trials are conducted to monitor for unintended effects and assess the long-term impact of genetic alterations. Oversight from regulatory bodies and bioethics committees is vital to safeguard against misuse and to establish ethical guidelines for the responsible use of gene editing.
What is the difference between somatic and germline gene editing in CRISPR?
Somatic gene editing involves making changes to the DNA in body cells, affecting only the individual treated and not their offspring. Germline gene editing, on the other hand, involves changes to sperm, eggs, or embryos, which would be passed on to future generations. This distinction is crucial in discussions around the ethics and implications of gene editing technologies like CRISPR.
| Key Points | Details |
|---|---|
| Ethical Dilemmas | CRISPR gene editing raises questions about the morality of changing human differences. |
| Potential Benefits | CRISPR can potentially cure genetic diseases, such as sickle cell anemia. |
| Economic Considerations | The cost of CRISPR treatments can be exorbitant, leading to concerns over equity. |
| Oversight Issues | Lack of international regulation on gene editing could lead to dangerous applications. |
| Unintended Consequences | Editing genes may result in unforeseen health effects, as genes interact in complex ways. |
Summary
CRISPR gene editing represents a groundbreaking advancement in medical science, allowing for the precise modification of genes to potentially eradicate debilitating diseases. However, the ethical implications of altering human genetics must be carefully weighed against its benefits. As discussions continue in the medical community, it is essential to consider the social, economic, and ethical ramifications of this powerful technology to ensure that it serves humanity as a whole.